Psychiatry should move away from unproven treatments, like it moved away from psychoanalysis.
Psychiatry hasn’t had the best reputation for a long time. The practice has sat under a cloud made up of poor understanding, stigma and many dangerous, often cruel treatments. Psychiatric patients are truly among the most vulnerable and underserved in the field of medicine, and many struggle on a daily basis. To make matters worse, there is a massive cadre of integrative practitioners, proponents, and related companies who are promoting and practicing what they call integrative psychiatry.
(Note that integrative psychiatry should not be confused with integrated psychiatry, which is merely the placement of psychiatrists into other patient care environments to increase access.)
A (very) brief history of mental illness

A trepanation hole, a prehistoric treatment for mental illness still used by some who should know better, today.
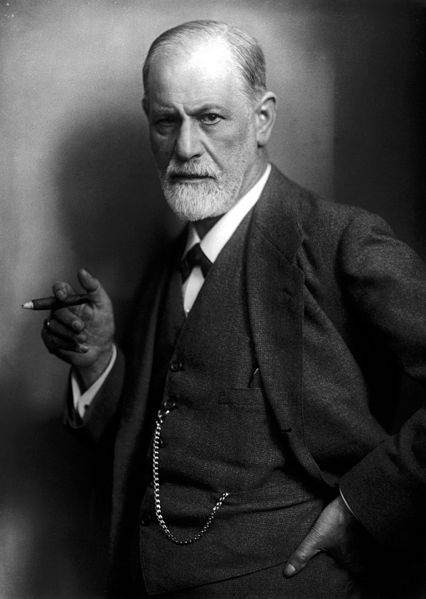
From ancient times until the middle of the 20th century there have been numerous pseudo-psychiatric treatments based upon religion, superstition and/or poor science. These include trepanation – drilling holes in the skull to release evil spirits (still practiced by some, believed to increase blood flow); exorcisms – also to rid the body of spirits; insulin shock therapy that would induce hypoglycemic comas; and the infamous lobotomy (leucotomy), which surgically isolated the prefrontal cortex. Antonio Moniz controversially received the Nobel Prize for the latter in 1949. However, for many conditions, the only treatments were psychoanalysis and far too often, long-term confinement in institutes across countries, some used for centuries (a few still exist as modern hospitals).
In the 1950s major psychiatric medications were introduced to the field: chlorpromazine, the first anti-psychotic, and imipramine, the first antidepressant; many others followed quickly. Through this new- found ability to control conditions, patients gained better control of their lives. A large movement of deinstitutionalization followed in the 60s, moving care from institutes to local centers and private practice. Psychiatry became more mainstream very quickly, consultations occurred more, and people became less afraid of the profession and its treatments. In the following decades further advances were made with the increased usage of the more recent benzodiazepines to replace the more dangerous barbiturates, and SSRIs to replace tricyclics and MAO-inhibitors, that often came with severe side effects and sometimes severe lifestyle restrictions, to treat depression. The asylum and lobotomy days are fortunately behind us, though there still exists a need for psychiatric hospitals and in unique, resistant cases the use of older drugs, electro-convulsive therapy, and sometimes involuntary admittance.
Though compared to the past the contemporary treatment of mental illness is far more advanced and humane, there are still major issues. The medications available are far from perfect. Research funding in the field typically falls far behind that of other diseases, and undertreatment is still a significant problem. The WHO estimates that more than 300 million people suffer from depression worldwide. With less than 50% treated (imagine that for other possibly fatal diseases), it is the current leading cause of disability worldwide. That is just depression though; if we were to factor in the number of people suffering from other mental illness in the world the number would likely be over a billion. With these numbers it must also be noted that the suffering endured is truly immeasurable; as a result, a patient’s desire for help is often just as great as those with cancer or other serious illnesses. Their mental states, often already fragile, unfamiliarity with mental illness, and desperation will allow predispose them to grasp at any hope, and integrative medicine stands ready to offer the illusion of a helping hand. Psychiatric illness is serious and should be taken seriously by society. Patients need science-based psychiatry, not more delusions.
Integration of CAM I – The nonsense
The methods employed by integrative psychiatry, like integrative medicine, can be roughly divided into two types: re-branding conventional advice as “alternative”, and promoting unproven and unscientific treatment options. Many of the purported treatments will be familiar to regular readers and well-researched medical sceptics, but there are a few that are quite rare and fringe, even in CAM. Integrative psychiatry doesn’t have any true centralization by itself like functional medicine does. As a result, practitioners fall under the broad aegis of integrative medicine, each choosing any point on the spectrum they like and defining the practice as they see fit.
The 2015 copy of Kaplan & Sadock’s Synopsis of Psychiatry (not to be confused with their Comprehensive Textbook of Psychiatry) has a chapter on CAM treatments. The book, and its ten prior editions, are mainstream and commonly used for education and reference. In the chapter devoted to CAM and integrative psychiatry, it has an extensive list of CAM options, and here I have excerpted some of the more obscure interventions, with a brief description:
- Anthroposophically extended medicine: using “wisdom of life” to perform mental exercises that balance mind and body
- Bates method: purportedly cures vision problems by splashing warm and cold water on the eyes, swaying, focusing on objects and thinking happy thoughts
- Trager method: sitting in a chair for an hour or so and being guided through the unconscious mind choosing its own better movements
- Environmental medicine: concerns about hypersensitivity and disease caused by electricity, wifi, etc. (note that there is also science-based environmental medicine and this ain’t it)
- Ozone therapy: introducing ozone (O3) to the body in order to treat everything from cancer to AIDS. It includes drinking ozonated water and “…insufflations, in which a catheter is inserted into the rectum or vagina with ozone administered at a slow flow rate; and autohemotherapy, in which a person’s own ozonized blood is reintroduced into the body.”
- Past life medicine: Using hypnosis to regress a person to a past life and “…the healing process is aided by contact with spiritual beings that are believed to have the ability to reverse illness and maintain health”; according to the text it is up to the psychiatrist to take the actual regression literally or figuratively
The list also includes many more, like acupuncture, chelation, chiropractic, colonic irrigation, homeopathy, naturopathy, therapeutic touch, and even shamanism.
Integration of CAM II – The rebranding
As far as rebranding is concerned, there is quite a bit – such as listing exercise as a CAM modality, as is often seen in similar writing. Tai chi and yoga are also listed separately even though they are just other forms of exercise. Nutrition is also listed as alternative, but criticizes the USDA guidelines and gives fad diets like the Atkins and Ornish diets as examples of “alternative diets”. Strikingly, the use of B-vitamins in alcoholics is also listed as alternative when it has been standard care for a while.
Biofeedback and hypnosis were not on the full list because these “modalities” are now “incorporated into standard psychiatric practice.” Both are umbrella terms that can cover many things, but neither are truly commonplace in psychiatry. Biofeedback has been experimented with by multiple fields of medicine, including psychiatry for some time now. It is, put simply, using a machine interface to provide perceptible readings on normally imperceptible bodily processes (such as blood pressure, skin conductance, or brainwaves) in an attempt to help patients monitor and control them in some way. There is evidence both for and against the intervention but considering the many different forms it can take it seems inappropriate to give such a blanket endorsement of the practice.
Hypnosis, on the other hand, is partly approved of by both the American Psychiatric Association [PDF] and the American Psychological Association. These endorsements are not, however, a blanket approval of all forms of the therapy. In fact, along with other medical organizations they condemn the practice of regression therapy with the aim of recovering repressed memories, because the likely result is actually the implantation of false memories, many taking the form of alien abductions, satanic ritual abuse, and sexual abuse. Integrative psychiatry, on the other hand, considers it to be a useful tool and encourage its use.
It may appear that the list of interventions was put in place simply to inform readers of the various forms of CAM and wasn’t an approval, but the sentence that follows the section implies otherwise:
Any of the complementary methods described in this section can be integrated into standard psychotherapeutic practice, although some lend themselves better than others.
These treatments don’t simply reside in ink though, they are in actual practice. A quick google search will reveal a tremendous number of doctors offering integrative psychiatric care, many offering phone consultations. It is likely that you can shop around for just about any alternative treatment you would like and get someone with a medical degree to condone it. This movement isn’t confined to small and individual practices, though; the Wellness Institute at the Cleveland Clinic (yes, that Cleveland Clinic) offers holistic psychotherapy that may consist of regression hypnosis, breath therapy that utilizes vibrational energy, guided imagery, and rebirthing breath that can help overcome the previous trauma of birth. UCSF offers acupuncture and ayurvedic massage among other things. It also seems that integrative psychiatry is buying into unproven diagnoses: ILADS (yes, that ILADS) has produced its own pamphlet for psychiatrists, in which it shows that nearly all psychiatric symptoms can be caused by chronic Lyme disease (yes, that chronic Lyme disease!) and mentions of it can be found on many websites.
Keeping with the forward march of CAM into mainstream medicine, the American Psychiatric Association has a dedicated “sub-specialty” devoted to integrative psychiatry. They offer a CME course through their online education center, and various webinars, and their publishing arm offers multiple books on the subject (this is the same organization that publishes the DSM).
Conclusion: Psychiatry needs more science, not less
It isn’t unfair to say that psychiatry is far from the most science-based specialty in medicine (a problem it shares with psychology and psychotherapy). The causes of many conditions are not known, and most hypotheses as to what does cause them are largely based on what effects psychiatric medications have inside the body. Researchers are working diligently in multiple fields to understand the genetic, environmental, and social causes of mental illness. Amazing progress has been made and there is a lot to come, but just because the train of science moves slowly does not give a reason to hang off the side and pick up magical cures along the track. Mental illness can often be severe and debilitating. It contributes greatly to shortened life spans, poverty, and global economic loss. It therefore must be taken extremely seriously. It is difficult now to get even basic treatment to half the people that require it. The solution requires a massive expansion of funding, outreach, and social awareness.
Adding unrealistic and fictional interventions to the field will only cause harm, and in my opinion it seems cruel for psychiatrists to be putting delusions into the heads of patients with mental illnesses. This can only be stopped through the work of an informed public. If these treatments were to enter the mainstream in significant amounts, it would be extremely difficult to push them back out. Nothing is without risk, and the risks present are simply too large. It is easy to imagine a patient with schizophrenia or depression that gets the idea their conditions can be treated simply and without medications that often come with adverse effects, especially when medication compliance is already a serious challenge in the field. Modern psychiatry isn’t great, but it helps and it is far better than what we used to have — but that’s the direction integrative psychiatry moves, towards pseudo-science and superstition harkening back to a time when psychiatrists treated their patients on personal whims and theories with no true regard for the patient. As a patient with depression and anxiety I want real science-based psychiatry, not to be propped up by a placebo that could shatter at any moment with possibly disastrous results.
